
(715)372-5590
www.northlandvet.net
|
In animals with reduced cobalamin absorption, regardless of the cause, it is reasonable to expect that eventual depletion of cobalamin body stores will occur and cobalamin deficiency will ensue. As all cells in the body require cobalamin for single carbon metabolism, it has been hypothesized that cobalamin deficiency may actually contribute to the clinical signs and manifestations of gastrointestinal disease in some patients. Studies of radiolabelled cobalamin in cats have demonstrated that the half-life of this compound is significantly reduced in cats with gastrointestinal disease. While the serum concentration of cobalamin is used diagnostically, the reactions catalyzed by cobalamin dependent enzymes occur in the mitochondria, making it difficult to assess the state of cobalamin availability in the patient. Tissue-level deficiency of cobalamin is associated with an increase in the urinary and serum concentrations of an organic acid called methylmalonic acid, which is an alternative product of a cobalamin dependent pathway within the mitochondria. Using this compound as a marker of cobalamin deficiency, we have been able to demonstrate that cats and dogs with very low serum cobalamin do indeed have a significant tissue-level cobalamin deficiency (Figure 2). Interestingly, in cats, there was no change in serum concentrations of homocysteine (see Figure 1). Elevation in homocysteine is expected with cobalamin deficiency due to reduced methionine synthase activity even in the face of extreme cobalamin deficiency. In dogs, preliminary evidence suggests that there is an increase in serum homocysteine concentration with reduced serum cobalamin concentration. 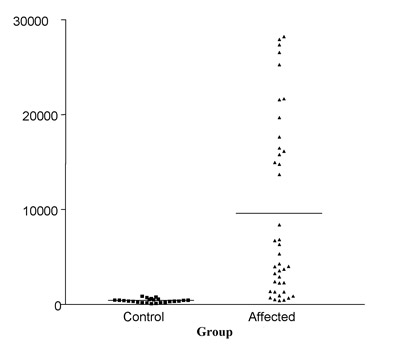
Cobalamin TherapyAs described above, there is compelling evidence that significant tissue-level cobalamin deficiency is present in some companion animal patients with gastrointestinal disease. The significance of this finding for the clinical management of these patients is also becoming clearer. A recent study has examined the effect of cobalamin supplementation on the outcomes of treatment for feline patients with severe cobalamin deficiency and histories suggesting chronic gastrointestinal disease.5 In this study, serum concentrations of methylmalonic acid normalized following parenteral cobalamin supplementation, indicating that cobalamin deficiency was the cause of the high methylmalonic acid in serum. There was an overall weight gain in these patients and a decrease in the frequency of clinical signs such as vomiting and diarrhea. During the course of the study, there was no change to the therapeutic regime other than the introduction of parenteral cobalamin supplementation. Dogs with exocrine pancreatic insufficiency will commonly present with subnormal serum cobalamin concentrations. Therapy with bovine pancreatic enzyme extracts is not sufficient to restore cobalamin absorption in dogs with EPI, as intrinsic factor appears to be species-specific. Failure to absorb cobalamin in dogs with EPI may be due to all three potential causes of low serum cobalamin. The pancreatic secretion of intrinsic factor is reduced or absent, secondary dysbiosis of the intestine is common, and the mucosa may be compromised by the presence of excessive bacterial numbers and toxic metabolites. Dogs with exocrine pancreatic insufficiency should be considered at high risk for the development of cobalamin deficiency. As clinical signs of cobalamin deficiency include chronic wasting or failure to thrive, malaise, and gastrointestinal signs such as diarrhea, serum cobalamin concentration should be measured in any dog with poor response to enzyme replacement therapy for EPI. Cobalamin should be supplemented whenever serum cobalamin concentration is in the low normal range (i.e., less than approximately 400 ng/L) in both dogs and cats. Most commonly, cyanocobalamin is chosen for supplementation, as it is both widely available and inexpensive. Very little evidence-based information about the route and dose of cobalamin supplementation in dogs and cats is available. Recent studies in humans, dogs, and cats suggest that oral supplementation is as equally effective as parenteral supplementation. We currently recommend either oral or parenteral cobalamin supplementation and the recommended protocol and dose for each route is as below. For oral cobalamin supplementation: Protocol: Daily administration for a total of 12 weeks and re-check the serum cobalamin concentration 4 weeks after stopping supplementation. The need for continued supplementation (and if so, the dose and frequency) can be reassessed at this time. (Dependent on patient's needs) Dose: 250 µg (also known as micrograms(mcg))in cats and 250 – 2000 µg (also known as micrograms (mcg))in dogs, depending on the size of the patient:
For parenteral cobalamin supplementation: Protocol: weekly injections for 6 weeks, then one dose a month later, and retesting one month after the last dose( dependent on patient's needs) For either oral or parenteral supplementation, if the underlying disease process has resolved and cobalamin body stores have been replenished, serum cobalamin concentration should be supranormal at the time of reevaluation. However, if serum cobalamin concentration is within the normal range, treatment should be continued at least monthly (for parenteral supplementation) and the owner should be forewarned that clinical signs may recur sometime in the future. Finally, if the serum cobalamin concentration at the time of reevaluation is subnormal, further work-up is required to definitively diagnose the underlying disease process and cobalamin supplementation should be continued weekly or bi-weekly (for parenteral supplementation) or daily (for oral supplementation). Dose: SC injection of 250 µg per injection in cats and, 250-1500 µg per injection in dogs, depending on the size of the patient:
*Information provided by Texas GI Lab* |